Pulmonary Function Tests
Pulmonary Function tests measures the function of lung capacity and lung and chest wall mechanics to determine whether or not the patient has a lung problem. Pulmonary Function Tests are commonly referred to as “PFTs”. When a patient is referred for PFT’s, it means that a battery of tests may be carried out, including simple screening spirometry, static lung volume measurement, diffusing capacity for carbon monoxide, airways resistance, respiratory muscle strength, and arterial blood gases.
Pulmonary Function Tests are used for the following reasons:
- Screening for the presence of obstructive and restrictive diseases
- Evaluating the patient prior to surgery – this is especially true of patients who:
- are older than 60-65 years of age
- are known to have pulmonary disease
- are obese (as in pathologically obese)
- have a history of smoking, cough, or wheezing
- will be under anesthesia for a lengthy period of time
- are undergoing an abdominal or a thoracic operation
- Evaluating the patient’s condition for weaning from a ventilator. If the patient on a ventilator can demonstrate a vital capacity (VC) of 10 – 15 ml/Kg of body weight, it is generally thought that there is enough ventilatory reserve to permit (try) weaning and extubation.
- Documenting the progression of pulmonary disease – restrictive or obstructive
- Documenting the effectiveness of therapeutic intervention
Forced Vital Capacity (Dynamic)
Flow volume loops are perhaps the most recognizable of all pulmonary function tests. The shape of the curves are extremely diagnostic but the very nature of the effort required to reproduce the shape (loop) means that often data is of poor quality. In ComPAS2 we have gone to extraordinary lengths to help the technician acquire high quality clinical data. Each of the test efforts is automatically reviewed against ATS standards and furthermore a “confidence” rating is applied by an even stricter performance scan utilizing Morgan Scientific experience.
In most pulmonary function labs, flow volume loops are usually the first tests gathered from the spirometry testing. By examining the information and shape of the loop, it helps clinicians further understand the way air is moving into and out of the lungs and help identify specific diseases that can otherwise be very hard to diagnose.
From the information gathered with this test certain deductions about what is happening throughout the lung can be made. In particular we comment on obstructive lung disorders and degree of the disease. Obstructive lung disease is simply put, a problem with the airways that do not allow airflow to move smoothly from the alveoli (air sacs of the lungs) and smallest airways out through the trachea (main windpipe) and ultimately out through the mouth when exhaling or inhaling. There are a number of common processes that can lead to this kind of a problem including emphysema, asthma and chronic bronchitis.
The results of dynamic pulmonary function tests place patients in 1 of 3 categories:
- normal lung function
- obstructive disease
- or restrictive disease
In obstructive lung disease, patients have decreased airflow (decreased FEV1/FVC ratio) and usually have normal or above-normal lung volumes.
In restrictive lung disease, patients have decreased lung volumes or TLC with normal airflow (normal FEV1/FVC ratio but with reduced values for both FVC and FEV1 individually).
For many years, the forced expiratory effort was only represented as a plot of volume against time.
Identifying Measurements on the Forced Expiratory Maneuver
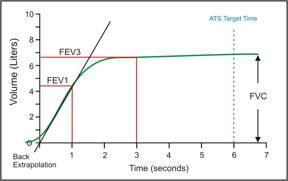 Forced Vital Capacity (FVC) is the maximum volume of air which can be exhaled or inspired during a forced (FVC) maneuver. For the tests to be of significance, it is recommended that the forced effort be 6 seconds or longer in duration.
Forced Vital Capacity (FVC) is the maximum volume of air which can be exhaled or inspired during a forced (FVC) maneuver. For the tests to be of significance, it is recommended that the forced effort be 6 seconds or longer in duration.
In most cases, the SVC is always greater than FVC. As more obstruction is present in the lungs the difference between SVC and FVC is more pronounced.
Forced Expired Volume in one second (FEV1) is the volume expired in the first second of maximal expiration after a full inspiration and is a useful measure of how quickly the lungs can be emptied.
FEV1/FVC is the FEV1 expressed as a percentage of the FVC and gives a clinically useful index of airflow limitation.
The forced volume excursion when plotted against flow rate reveals perhaps the most recognizable shape in pulmonary function testing. There are many measurements that can be taken from this single dynamic effort.
Identifying Measurements on the Flow Volume Loop
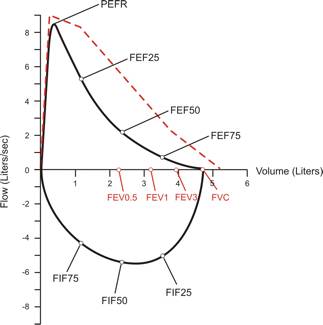 Peak Expiratory Flow Rate (PEFR). The first landmark reached is the PEFR. The first blast of air exhaled from the patient reaches this flow rate almost immediately. The flow rate then quickly slows as more air is exhaled. This landmark is very important in judging if the patient is giving maximal effort, overall quality of the test, strength of expiratory muscles, and the condition of the large airways, such as the trachea and main bronchi.
Peak Expiratory Flow Rate (PEFR). The first landmark reached is the PEFR. The first blast of air exhaled from the patient reaches this flow rate almost immediately. The flow rate then quickly slows as more air is exhaled. This landmark is very important in judging if the patient is giving maximal effort, overall quality of the test, strength of expiratory muscles, and the condition of the large airways, such as the trachea and main bronchi.
Forced Expiratory Volume after 0.5 seconds (FEV0.5). The FEV0.5 indicates the amount of air exhaled with maximum effort in half a second.
Forced Expiratory Volume after 1 second (FEV1). The FEV1 indicates the amount of air exhaled with maximum effort in the first second. The FEV1 is another very important landmark in assessing the overall status of the patient and quality of the test. This test result is also important in pre- and post-bronchodilator tests in determining the effects of bronchodilators on the airways.
Forced Expiratory Volume after 3 seconds (FEV3). The FEV3 indicates the amount of air exhaled with maximum effort in the first three seconds.
Forced Expiratory Volume after 6 seconds (FEV6). The FEV6 indicates the amount of air exhaled with maximum effort in the first six seconds. This parameter is primarily used to ensure expiratory efforts meet or exceed 6 seconds.
Forced Vital Capacity (FVC). Another important result of a Flow Volume Loop is the FVC. Many of the other results depend on this number. The FVC is the total volume of air exhaled with maximal effort.
Forced Expiratory Flow at 25% of FVC (FEF25%). The FEF25% is the flow rate at the 25% point of the total volume (FVC) exhaled. Assuming maximal effort this flow rate is still indicative of the condition of fairly large to medium size bronchi. This landmark is used in calculations with the FEF75% to give FEF25-75%, the middle half of the FVC, which many physicians look at as not being dependent on patient effort and an indicator for obstruction in the small airways. This value is very dependent on the total volume exhaled (FVC) and tends to be highly variable from test to test.
Forced Expiratory Flow at 50% of FVC (FEF50%). The FEF50% is the flow rate at the 50% point of the total volume (FVC) exhaled. This landmark is at the midpoint of the FVC and indicates the status of medium to small airways, it’s sometimes looked at instead of the FEF25-75%.
Forced Expiratory Flow at 75% of FVC (FEF75%). The FEF75% is the flow rate at the 75% point of the total volume (FVC) exhaled. This landmark indicates the status of small airways and is used in the FEF25-75% calculation. The damage done by most chronic pulmonary diseases show up in the smallest airways first and early indications of this damage begin to appear toward the end of the expiratory part of the Flow Volume Loop.
Forced Inspiratory Flow at 25% of FVC (FIF25%). The FIF25% is the flow rate at the 25% point on the total volume inhaled. The inspiratory flow rates are relatively unimportant in assessing the asthmatic. Abnormalities here are indicators of upper airway obstructions. Areas of the mouth, upper and lower pharynx (back of the throat), larynx (voice box), and vocal-cords impact the inspiratory flow rates.
Peak Inspiratory Flow Rate (PIFR). The fastest flow rate achieved during inspiration.
Forced Inspiratory Flow at 50% of FVC (FIF50%). The FIF50% is the flow rate at the 50% point on the total volume inhaled.
Forced Inspiratory Flow at 75% of FVC (FIF75%). The FIF75% is the flow rate at the 75% point on the total volume inhaled.
Some of the other numbers that can be calculated from the Flow Volume Loop are:
FEV1/FVC%, and FEV3/FVC% – These are ratios calculated by dividing the Forced Expiratory Volume results by the Forced Vital Capacity and expressed as a percentage of the FVC.
Forced Expiratory Time (FET) – The time it takes to exhale as much air as possible. To obtain reliable FVC values, the expiratory effort should be continued for at least 6 seconds. The FET should never be less than 6 seconds unless the patient is severely restricted.
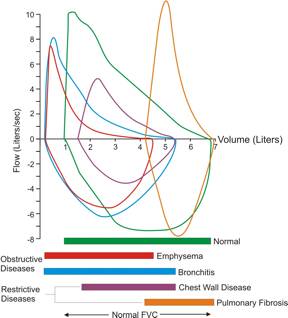 This illustration shows the variety of flow volume loop shapes that often relate to particular disease. When looked at in relation to the lung volume further clinical information can be revealed.
This illustration shows the variety of flow volume loop shapes that often relate to particular disease. When looked at in relation to the lung volume further clinical information can be revealed.
Slow Vital Capacity (Static)
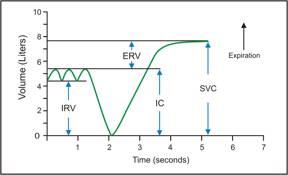
Slow vital capacity was arguably the first ever recorded lung volume. The full excursion of the maneuver gives a measure of the change in volume of gas in the lungs from complete inspiration to complete expiration or vice versa. The recording of volume versus time is called a spirogram. In the example shown, the recording begins with the subject quietly breathing in a steady-state condition followed by a maximal breath-in and a full breath-out. The spirogram of a slow vital capacity maneuver has several key identifying components.
Identifying the Sub-divisions of Slow Vital Capacity
Slow Vital Capacity (SVC) is the maximum volume of air which can be exhaled or inspired in a slow/steady maneuver.
Vital Capacity (VC) is the largest of the volumes from either a forced (FVC) or a slow (SVC) maneuver.
Expiratory Reserve Volume (ERV) is the maximum volume of additional air that can be expired from the end of a normal expiration.
Inspiratory Capacity (IC) is the maximum volume of air that can be inspired from end expiratory position. Called a capacity because it is the sum of 2 lung volumes: IC = IRV+TV
Maximum Voluntary Ventilation (Dynamic)
The volume of gas that can be breathed in 15 seconds when a person breathes as deeply and quickly as possible. Also called maximum breathing capacity. The result is extrapolated from 15 seconds to show what could be achieved over one minute. As a general guide, the value should correlate closely to the FEV1 x 35.
This test is usually performed whenever spirometry is done. If people have weakness in the muscle of breathing this test can help identify these difficulties. The MVV is a test of ultimate effort dependency and is often discarded by physicians. Since it has been shown that the FEV1 x 35 is a good indication of MVV, many centers simply report that result. Disability criteria however still require an actual MVV to be done!
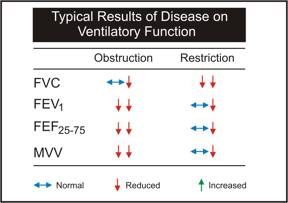
Chart Showing the Typical Results of Disease on Spirometry