By Jeffrey M. Haynes RRT RPFT FAARC
Three elements are required to obtain quality pulmonary function tests (PFTs): accurate instruments; capable and cooperative patients; knowledgeable and motivated technologists.
While instrument failures certainly can occur, properly maintained PFT equipment is not a common cause of poor quality data.
Patients are the frequently the scapegoat when test quality is subpar.
However, multiple studies have shown that the overwhelming majority of patients can perform PFTs correctly when properly coached.
For example, Enright et al[1] reviewed 18,000 consecutive spirometry tests in patients ages 20-90 years and found that 90% of the patients could produce high quality data.
While it is commonly believed that elderly patients can be expected to perform PFTs poorly, a study comparing PFT quality from 40-50-year-old patients and 80+ year old patients showed no difference. [2]
In fact, the most common cause of low quality PFTs is a poorly trained and/or unmotivated technologist.
The most effective tool to increase the quality of PFTs is a technologist performance monitoring and feedback program.
The Lung Health Study documented that after the initial training technologists, PFT quality progressively declined.
Technologist performance improved after re-training; however, high quality was only sustained following the implementation of a technologist performance monitoring and feedback program. [3]
Similar findings have been found in numerous epidemiologic studies.
In 2012 Borg et al[4] studied the effect of a technologist performance monitoring and feedback program in two clinical PFT laboratories.
At the beginning of the study the rate of ATS/ERS spirometry acceptability and repeatability was 61% in lab #1 and 59% in lab #2.
After this initial assessment lab #1 implemented a technologist performance monitoring and feedback program and lab #2 did not.
Four years after implementation of technologist performance monitoring the rate of ATS/ERS spirometry acceptability and repeatability in lab #1 shot up to 92% while lab #2 stayed at an unacceptable 65%.
The good news is that technologist performance monitoring is quick and easy to perform with ComPAS software.
Simply selected administrative reports under tools and select “technician proficiency (summary)” for report type.
Figure 1 shows my statistics in 2010 for spirometry and DLCO.
The solid green check mark indicates the number of acceptable and repeatable tests.
The open check mark indicates the number of tests in which acceptable tests were not repeatable.
The check mark with the circle-backslash symbol indicates the number of test in which no acceptable maneuvers could be captured.
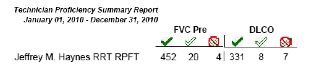
Figure 1. Technician proficiency report available in ComPAS.
Technologist performance monitoring is recommended by the ATS/ERS PFT guidelines.
If your lab is not monitoring technologist performance, can you really assert that your lab is compliant with ATS/ERS guidelines?
[1] Enright PL, Beck KC, Sherrill DL. Repeatability of spirometry in 18,000 adult patients. Am J Respir Crit Care Med. 2004;169(2):235-238.
[2] Haynes JM. Pulmonary function test quality in the elderly: a comparison with younger adults. Respir Care 2014;59(1):16-21.
[3] Enright PL, Johnson LR, Connett JE, Voelker H, Buist AS. Spirometry in the lung health study. 1. Methods and quality control. Am Rev Respir Dis. 1991;143(6):1215-1223.
[4] Borg BM, Hartley MF, Bailey MJ, Thompson BR. Adherence to acceptability and repeatability criteria for spirometry in complex lung function laboratories. Respir Care 2012;57(12):2032-2038.
